Bones, the structural backbone of our body, are susceptible to different types of fractures. Understanding these varieties is critical for effective treatment and swift recovery. In this guide, we delve into the types of fractures, their unique characteristics, and the advancements in their treatment.
Understanding Stress Fractures
Stress fractures represent a salient warning from our skeletal system, signaling that the endurance limits of our bones have been tested. Typically presenting as tiny, hairline breaks, stress fractures are the result of repetitive force, often from overuse — such as the repeated impact of feet hitting the ground in long-distance runners.
The Mechanics Behind the Injury
Bones are dynamic structures, constantly remodeling and adapting to stress. However, if the imposed stress exceeds the bone’s intrinsic ability to repair itself, micro-fractures can accumulate and eventually manifest as stress fractures. They most commonly affect weight-bearing bones, such as the tibia (shinbone), metatarsals (foot bones), and the femur (thighbone).
Risk Factors and Prevention
Certain factors can increase the risk of developing stress fractures, including:
-
- Intense training or a sudden increase in physical activity without proper conditioning.
-
- Inadequate nutrition, particularly calcium and vitamin D deficiencies, which weaken bone density.
-
- Specific foot conditions, like flat feet or high arches, that alter stress distribution during movement.
-
- Previous stress fractures, which can predispose the bone to subsequent injuries.
Preventive strategies are pivotal in mitigating the risk of stress fractures:
-
- Gradual progression in training intensity to allow bones to adapt.
-
- Cross-training to distribute the physical load across various muscle groups and bones.
-
- Ensuring a diet rich in bone-building nutrients, and in some cases, supplementation upon a doctor’s recommendation.
-
- Using proper footwear that provides support and cushioning to absorb shock.
Diagnosis and Treatment
Diagnosing stress fractures can be challenging, as they often elude detection on initial X-rays. Healthcare professionals may resort to MRI or bone scans for a definitive diagnosis, which are more sensitive in the early stages of the injury.
Once diagnosed, the primary treatment for a stress fracture is rest. The affected limb should be relieved of the load to facilitate healing. This might mean refraining from the activity that caused the injury for six to eight weeks or more, depending on the severity.
In addition to rest, treatment may include:
-
- Protective footwear or braces that shield the injured bone from stress.
-
- Physical therapy to maintain strength and flexibility in the surrounding muscles.
-
- Adjustments to exercise routines focusing on low-impact activities during the recovery phase.
Returning to Activity
The return to full activity after a stress fracture should be a gradual process. It’s crucial to allow the bone to fully heal and to address any contributing factors to prevent recurrence. Athletes should work closely with coaches and sports medicine professionals to tailor a safe return-to-play program.
Conclusion
While stress fractures are an occupational hazard for athletes, they can affect anyone who engages in repetitive physical activities. Understanding the delicate balance between activity and recovery is the key to maintaining strong, resilient bones and avoiding the pitfalls of overuse injuries.
Anatomy of a Compound Fracture
When the integrity of bone and skin is compromised simultaneously, it results in what is known as a compound fracture, also referred to as an open fracture. This type of injury is not just a break in the bone; it’s a break that communicates with the outside environment through a wound in the skin. Such fractures are considered serious because the open wound exposes the bone and deep tissues to potential contamination, raising the risk of infection and complex healing challenges.
The Mechanism of Injury
Compound fractures typically result from high-impact trauma such as vehicular accidents, falls from significant heights, or severe sports-related contact. The force is so overwhelming that it not only breaks the bone but also carries it through the soft tissues and skin.
Complications and Immediate Action
The exposed nature of compound fractures introduces the risk of infection, including the dreaded osteomyelitis — an infection of the bone. Other complications may include blood loss, nerve damage, and muscle injury. Immediate medical attention is crucial, with the first steps at the accident scene including:
-
- Preventing further contamination.
-
- Controlling bleeding.
-
- Immobilizing the affected limb.
Treatment: A Multidisciplinary Approach
The treatment of compound fractures requires a multifaceted approach:
-
- Surgical Intervention: Urgent surgery is often necessary to clean out debris from the wound (debridement) and to stabilize the fracture, typically using rods, plates, or screws.
- Antibiotics: To combat and prevent infection, broad-spectrum antibiotics are administered as soon as possible.
- Tetanus Prophylaxis: A tetanus shot is often required, especially if the wound is contaminated with soil or street dust.
- Wound Management: The wound requires regular, careful dressing changes and monitoring for signs of infection.
- Rehabilitation: Physical therapy is a critical component of recovery to restore function and strength.
Recovery and Outcomes
Recovery from a compound fracture can be a lengthy process, often taking longer than a simple fracture due to the need for wound healing and the potential for complications. Patient outcomes depend on several factors, including the severity of the fracture, the patient’s overall health, and the timeliness and effectiveness of the initial treatment.
Prevention and Education
Preventive measures for compound fractures are largely centered around safety precautions, such as using protective gear during high-risk activities and following workplace safety protocols. Public education on immediate care for such injuries can also play a role in improving outcomes.
Conclusion
Compound fractures pose a substantial challenge in orthopedic care, demanding prompt and comprehensive medical intervention. Through a combination of surgical expertise, rigorous infection control, and diligent rehabilitation, patients can overcome these complex injuries and regain much, if not all, of their pre-injury function.
Grasping the Gravity of Comminuted Fractures
Comminuted fractures occur when a bone is subjected to such high-impact energy that it shatters into three or more pieces. Unlike simple fractures where the bone may crack in one place, comminuted fractures involve multiple breaks that create several bone fragments. These injuries often result from severe accidents, such as those involving motor vehicles, falls from a great height, or direct blows in contact sports.
Complexities in Treatment
The complexity of comminuted fractures lies in the difficulty of restoring the original structure of the shattered bone. The primary goals in treating this type of fracture are to reconstruct the bone to its natural shape, ensure that the bone fragments are stable enough to heal, and re-establish the functionality of the affected limb.
A Multi-Stage Surgical Journey
Treatment often involves multiple surgeries:
- Initial Surgery: The first surgery may be to clean the wound (if open) and to piece together the bone fragments using fixation devices like wires, plates, screws, or rods.
- Secondary Procedures: Additional surgeries might be necessary to adjust the fixations or to perform bone grafting, where bone from another part of the body or a donor is used to repair the damaged area.
- Reconstructive Surgery: In some cases, reconstructive surgery is needed to restore the appearance and function, especially if the fracture is near a joint.
Innovation in Repair Techniques
Advancements in medical technology have introduced new materials and methods for treating comminuted fractures, such as:
- 3D Printing: Using patient-specific 3D models to plan surgery or even 3D-printed bone fragments for reconstruction.
- Biological Enhancements: Applying bone morphogenetic proteins (BMPs) that promote bone growth and healing.
- Minimally Invasive Techniques: Employing techniques that reduce the surgery’s impact on the body, leading to faster recovery times.
Rehabilitation: Regaining Functionality
Post-surgery, rehabilitation is crucial. A team of physical therapists and occupational therapists work together to develop a personalized plan to:
- Restore movement and strength.
- Reduce stiffness.
- Alleviate pain.
- Optimize the healing environment for the bone.
Challenges in Recovery
The road to recovery from a comminuted fracture can be arduous and lengthy. It requires not just physical healing but often psychological support to cope with the changes and limitations during the recovery period. The patient’s active participation in the rehabilitation process is vital to the success of the treatment.
Conclusion
Comminuted fractures represent a severe trauma to the skeletal system and pose significant challenges in orthopedic surgery and rehabilitation. With the right combination of surgical expertise, innovative treatment modalities, and comprehensive rehabilitation, patients can make significant strides towards regaining their mobility and quality of life.
Unraveling the Nuances of Hairline Fractures
Hairline fractures, often referred to as stress fractures, are small cracks in the bone that can be as deceptive as they are painful. They typically result from repetitive stress on the bone over time rather than from a single, acute incident. This type of fracture is common among athletes, dancers, and military recruits—essentially, anyone whose activities involve persistent impact on the feet and legs.
The Silent Onset
Unlike more dramatic and obvious breaks, hairline fractures can develop slowly, manifesting as a nagging pain that intensifies with activity and subsides with rest. Because of their subtlety, they are often misdiagnosed or overlooked in early stages, making awareness and early detection critical.
Identifying Hairline Fractures
Diagnosis of a hairline fracture is not always straightforward. Early X-rays may miss the small crack, and it may take a repeat X-ray weeks later, or the use of more sensitive imaging like an MRI or bone scan, to confirm the diagnosis.
Tailored Treatment for Recovery
The cornerstone of treating hairline fractures is rest. The affected limb often requires a period of immobilization from weight-bearing activities to give the bone time to heal. Treatment may also include:
- Protective footwear to redistribute pressure away from the fracture site.
- Adjustments to exercise routines, emphasizing low-impact activities during the healing process.
- Adequate nutrition, particularly calcium and vitamin D, to support bone healing.
A Patient’s Path to Healing
The healing process for a hairline fracture is a gradual one, with the timeline varying based on the fracture’s location and severity. Patience is paramount, as returning to high-impact activities too soon can lead to a full-blown fracture.
Preventive Measures
Prevention of hairline fractures is centered on understanding and respecting the body’s limits. Proper training techniques, appropriate footwear, and cross-training can help distribute the repetitive forces that cause these injuries. Listening to one’s body and seeking medical advice at the first sign of persistent bone pain can prevent a small crack from becoming a significant setback.
Conclusion
Hairline fractures may be subtle, but their impact on an individual’s activity level can be significant. With careful attention to the body’s warning signs, appropriate medical care, and a focus on proper recovery time, these minor fractures can heal completely, allowing individuals to return to their favorite activities without lasting consequences.
Decoding Simple Fractures
A simple fracture, also known as a closed fracture, is characterized by a singular, clean break in the bone with no open wound on the skin. These fractures occur when the bone is subjected to a force it cannot withstand, but unlike compound fractures, the skin remains intact. Simple fractures are common in everyday accidents, such as falls, direct blows, or sports injuries.
Symptoms and Diagnosis
Despite their straightforward nature, simple fractures can be quite painful and result in noticeable symptoms, including:
- Immediate and localized pain at the site of the fracture.
- Swelling and possible bruising.
- Inability to bear weight or use the affected limb normally.
- Visible deformity if the bone is displaced.
Diagnosis typically involves a physical examination followed by imaging tests. An X-ray is usually sufficient to confirm a simple fracture and determine its precise location and extent.
Approach to Treatment
The main goals when treating a simple fracture are to ensure the bone heals in the correct position and to restore function to the affected limb. Treatment options include:
- Immobilization with a cast or splint to keep the bone ends in place.
- Closed reduction, which is a manual manipulation to realign the bone if it is displaced.
- Pain management through medication and, if necessary, physical therapy to rebuild strength and mobility.
The Healing Journey
The healing process for a simple fracture is generally straightforward, with the bone typically knitting back together over the course of several weeks to months, depending on the fracture’s severity and the patient’s overall health. Adequate rest and adherence to a doctor’s advice are key to a smooth recovery.
Ensuring a Strong Recovery
To facilitate healing, patients are advised to:
- Follow weight-bearing restrictions to prevent further injury.
- Engage in rehabilitative exercises once the bone has sufficiently healed to prevent stiffness and muscle atrophy.
- Maintain a healthy diet rich in calcium and vitamin D to support bone health.
Prevention and Awareness
While accidents can happen to anyone, certain measures can help prevent simple fractures:
- Wearing appropriate protective gear during sports and high-risk activities.
- Keeping living spaces free of tripping hazards.
- Strengthening bones through regular exercise and a balanced diet.
Conclusion
Simple fractures, although less complex than other types of bone breaks, require careful medical attention to heal properly. With appropriate treatment and a patient-centered approach to recovery, individuals can expect to return to their daily routines with full functionality restored in the affected limb.
The Sudden Snap of Avulsion Fractures
An avulsion fracture occurs when a sudden and forceful pull on a tendon or ligament—which is attached to a bone—results in a piece of the bone being torn away. Common in sports and high-impact activities, these fractures often happen during rapid acceleration or deceleration movements, when the force exerted by the contracting muscle exceeds the strength of the bone attachment.
Identifying the Injury
The telltale signs of an avulsion fracture include:
- Sharp, localized pain at the site of the injury.
- Swelling and bruising.
- Difficulty moving the affected limb or joint.
- Sometimes, a noticeable gap where the muscle has pulled away from the bone.
These fractures are typically diagnosed through physical examination and imaging tests, such as X-rays, to visualize the bone fragment pulled from its normal position.
Tailored Treatments for Optimal Healing
Treatment of avulsion fractures depends on the size of the bone fragment and the degree of displacement:
- Non-Surgical Management: If the bone fragment is not significantly displaced, treatment may involve rest, ice, compression, and elevation (RICE), alongside immobilization with a cast or splint.
- Surgical Intervention: When the fragment is large or displaced, surgery may be required to reattach the bone to its proper place with screws or pins.
Navigating the Recovery Process
Rehabilitation is key to recovery, often involving:
- Gradual exercises to restore range of motion.
- Strengthening exercises once the bone has healed.
- Physical therapy to ensure proper joint function and prevent stiffness.
Risks and Prevention
Athletes, particularly those in sports requiring quick starts or stops like soccer or basketball, are at higher risk for avulsion fractures. Preventive measures include:
- Proper warm-up and stretching before activity.
- Strength training to improve muscle and tendon resilience.
- Gradual increase in activity intensity to allow the body to adapt.
Conclusion
While avulsion fractures are less common than other types of breaks, they are nonetheless a serious injury that can significantly impact athletic performance and daily activities. Understanding the mechanism of injury and appropriate treatment options is essential for a full recovery and return to peak functionality.
Unveiling Pathological Fractures
Pathological fractures are bone breaks that occur as a result of an underlying medical condition which weakens the bone, rather than a specific injury or trauma. These conditions can include osteoporosis, bone cancer, or other diseases that affect bone density and strength. Understanding and managing these fractures require a careful consideration of both the fracture itself and the underlying health issue.
Detecting the Hidden Weakness
Symptoms of a pathological fracture may mirror those of other fractures — sudden pain in the affected area, swelling, and reduced function. However, the cause is not a recent injury but a bone compromised by disease. Diagnostic imaging, alongside a full medical assessment, is necessary to identify the fracture and understand its root cause.
Addressing the Fracture and Its Cause
Treatment for pathological fractures involves a two-pronged approach:
- Stabilizing the Fracture: This may include the use of casts, braces, or surgical intervention with pins, plates, or screws to stabilize the bone.
- Treating the Underlying Condition: A comprehensive treatment plan to address the underlying condition is critical. This might involve medications, lifestyle changes for diseases like osteoporosis, or more complex treatments for bone cancer, including chemotherapy, radiation, or targeted therapy.
The Recovery Equation
The recovery from a pathological fracture can be more complex due to the pre-existing bone weakness. Rehabilitation efforts focus on:
- Encouraging bone healing and strength through nutrition and appropriate therapies.
- Avoiding additional stress on the bones to prevent further fractures.
- Adapting physical activity to maintain mobility while minimizing fracture risk.
Prevention and Monitoring
Preventive strategies are key, especially for individuals at risk of bone-weakening conditions:
- Routine bone density screenings for early detection of osteoporosis.
- Nutritional adjustments to ensure adequate calcium and vitamin D intake.
- Exercise programs designed to enhance bone strength without overexertion.
Conclusion
Pathological fractures are a unique challenge in the realm of orthopedics, intertwining the need for acute fracture management with the complexities of chronic disease. With an individualized treatment plan that addresses both the fracture and its underlying cause, patients can achieve the best possible outcomes, maintaining their quality of life and bone health.
Understanding Greenstick Fractures
Greenstick fractures are unique injuries typically found in pediatric patients. Named for the way young, green branches can break—splintering but not severing completely—these fractures occur because children’s bones are more flexible compared to adults’. A greenstick fracture is characterized by a bend on one side of the bone and a break on the other, often resembling a partial crack.
Causes and Symptoms
These fractures commonly result from falls or sudden impacts that would cause a complete break in an adult bone. Symptoms mirror those of other fractures, such as:
- Pain at the site of the fracture.
- Swelling and tenderness.
- Obvious deformity, like a bend in the limb.
- Difficulty using or moving the affected limb.
Diagnosis and Treatment
Diagnosing a greenstick fracture involves a physical examination and imaging tests, most commonly an X-ray. Treatment focuses on realigning the bone if it’s bent and then immobilizing the limb to allow the bone to heal properly. This typically involves:
- A cast or splint to keep the bone in place.
- Possible gentle manipulation to straighten the bone if necessary, known as a reduction, which is usually less invasive than for complete fractures.
Healing and Recovery
Children’s bones heal faster than those of adults, so the recovery time from a greenstick fracture can be comparatively quick. Follow-up appointments are crucial to ensure the bone is healing in the correct alignment. During healing, it’s essential to limit activities that could re-injure the bone.
Preventive Measures and Education
Preventing greenstick fractures centers around creating safe environments for children and teaching them safe practices during play and sports. Use of appropriate safety gear, like wrist guards or helmets, can also reduce the risk of such fractures.
Conclusion
Greenstick fractures, while typically less severe than complete fractures, require prompt and appropriate treatment to prevent future complications such as growth disturbances or deformities. With proper care and attention to healing, children with greenstick fractures can expect to return to their playful and active lives with resilience and strength.
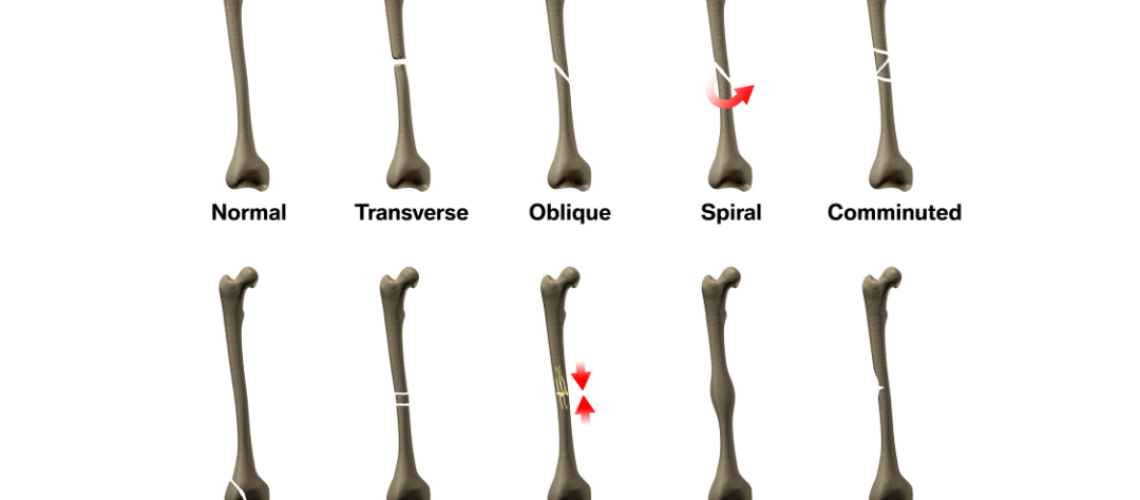
The Straightforward Nature of Transverse Fractures
Transverse fractures occur when a bone breaks in a straight line across. This type of fracture is typically the result of a force applied perpendicularly to the bone’s axis, such as a direct blow or a fall from a height. The clean, horizontal nature of the break is its defining characteristic, which can sometimes make it more stable and easier to treat than other fracture patterns.
The Angled Complexity of Oblique Fractures
Oblique fractures, in contrast, feature a diagonal break and often happen due to an angled impact or a combination of twisting and compression forces. The fracture line runs at an angle across the bone, making it more unstable and prone to displacement compared to transverse fractures.
Symptoms and Identification
Both transverse and oblique fractures share common symptoms with other types of bone breaks:
- Sudden onset of pain at the site of impact.
- Visible swelling and bruising.
- Difficulty bearing weight or using the affected part of the body.
- Deformity, particularly if the bone fragments have shifted.
Diagnosis for these fractures typically involves an X-ray to confirm the fracture type and assess the extent of the break. In some cases, additional imaging like CT scans might be necessary for more complex oblique fractures.
Treatment Protocols
The treatment for transverse and oblique fractures depends on the alignment of the bone fragments and the severity of the break:
- Closed Reduction and Immobilization: Non-displaced or minimally displaced fractures can often be treated with a cast or brace after a closed reduction, where the bone fragments are manually realigned.
- Surgical Intervention: More severe fractures, especially displaced oblique fractures, may require surgery for internal fixation using plates, screws, or rods to ensure proper healing.
Recovery and Rehabilitation
Healing times vary, but typically it takes several weeks for the bone to knit back together. Rehabilitation may involve:
- Physical therapy to restore strength and mobility.
- Gradual reintroduction to weight-bearing activities.
- Regular follow-up appointments to monitor the healing process through X-rays.
Prevention and Precaution
Preventative measures for transverse and oblique fractures are similar to those for other fractures and include:
- Using protective gear during high-risk activities.
- Ensuring safe environments to prevent falls.
- Maintaining bone health through nutrition and exercise.
Conclusion
Transverse and oblique fractures represent two of the more common fracture patterns encountered in orthopedic practice. Whether a straight-line break or an angled one, proper medical evaluation and treatment are crucial for a full recovery. Understanding these types of fractures and their specific challenges is key to effective management and ensuring patients can return to their daily activities without lasting impact.
Treatment and Healing: A Multifaceted Approach
The treatment of fractures is tailored to the type of break. While a simple fracture may need only a cast or splint, more complex fractures like comminuted or compound may require surgical intervention with hardware like rods, screws, or plates to maintain bone alignment during healing.
Rehabilitation plays a critical role in recovery. It begins with gentle movements and progresses to more strenuous activities that promote strength, flexibility, and function. Nutrition, including adequate calcium and vitamin D intake, also supports bone repair.
Conclusion
The world of fractures is as varied as the bones they affect, and the treatment as nuanced as the types of breaks that occur. Advances in orthopedic medicine continue to improve the prognosis for those suffering from fractures. Understanding these types of injuries is the first step towards a successful recovery and returning to the rhythm of daily life.